Syphilis
Syphilis is a sexually transmitted disease that has a tumultuous history and has been a threat since at least the 15th century. In the absence of definite answers, there are two main theories that try to explain its origin.
The first, called Colombian, claims that the disease originated in the Americas and was transported to Europe following the expeditions of Christopher Columbus. The pre-Columbian theory, on the other hand, holds that the disease was already present in the Old World, but developed into a more virulent form at the turn of the 15th and 16th centuries (which would explain the absence of traces prior to this period).
Throughout its long history it has had different names, typically related to the stigmatization of enemy populations. In Italy, from the year Charles VIII invaded (1494), syphilis was known as “French disease” while in France it was known as the “Neapolitan disease”. In Spain it was called the “German disease”, but the Danish, the Portuguese and the inhabitants of Northern Africa attributed it to the Spanish whereas the Turks coined the term “Christian disease”. The present name dates back to 1530 and was introduced by the Veronese poet and physician Girolamo Fracastoro.
CAUSES
Syphilis is a bacterial infection caused by the bacterium Treponema pallidum, a subspecies of Pallidum, which appears under the microscope as a small, spiral-shaped filament.
The natural history of syphilis is that of a chronic infection that can cause a series of highly variable clinical manifestations during the first 2-3 years of infection, followed by a typically prolonged latent stage that can evolve into years of clinically evident tertiary infection stage or even decades after initial infection.
Because syphilis lesions are often asymptomatic and can occur in regions of the body where they might go undetected, not all infected people show the classic signs of one or more clinical stages of infection. The disease is only sexually contagious during the early, primary, and secondary stages; however, congenital transmission can occur years after the start of latency.
TRANSMISSION
Infection occurs primarily as a result of unprotected sex, either genital or oral, with an infected person.
Passage can also occur via the tansplacental route, with vertical transmission from mother to child during pregnancy. Cases of indirect transmission or through transfusions are rarer.
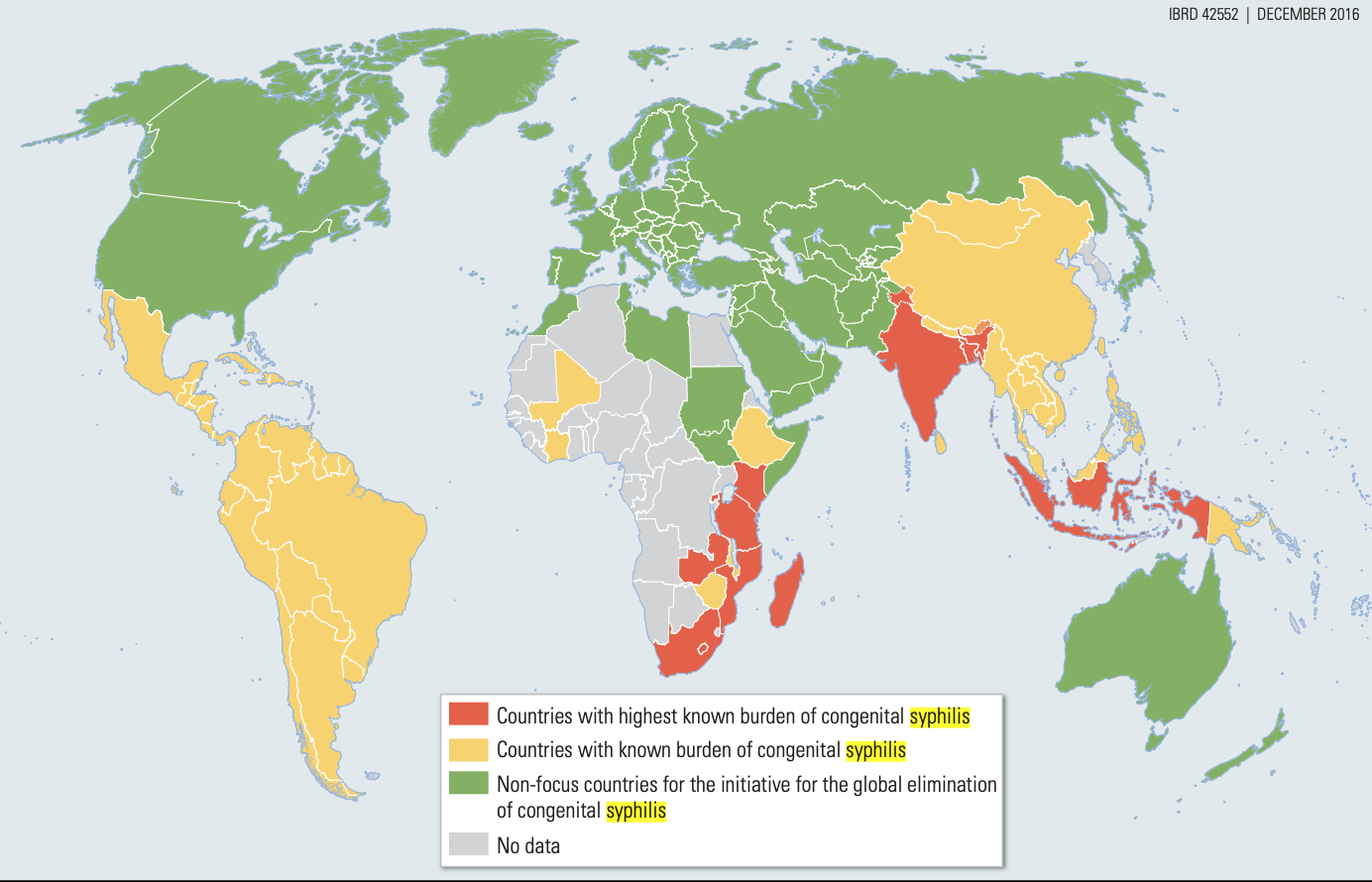
GEOGRAPHICAL DISTRIBUTION
More than 5 million new cases of syphilis are diagnosed worldwide each year, most of which occur in low-income countries where both endemic and uncommon congenital cases are found. Those affected include ordinary travellers who engage in different sexual behaviour during holidays or business trips, bringing home with them diseases for which they were not prepared.
In low- and middle-income countries, syphilis infection is a relatively common disease that is a source of substantial morbidity, including adverse pregnancy outcomes and accelerated HIV transmission.
In high-income countries, syphilis is largely transmitted within tight sexual and social networks. Although the disease is relatively rare, more than 15-20% of the U.S. population diagnosed had been infected well before diagnosis.
Although syphilis is a chronic infectious disease that could cause morbidity throughout its natural history, the infection is transmissible (with the exception of congenital infection) only in the early years of its course. For this reason, public health focuses its efforts on the primary, secondary and latent stages of infection, also referred to as infectious syphilis.
After two or three years without any treatment, infection is rarely transmitted sexually, but its range shifts to personal morbidity, resulting in late neurosyphilis and cardiovascular infections.
SYMPTOMS
First stage
In primary syphilis, the main clinical manifestation is the presence of an ulcerated lesion that typically appears about 2 to 3 weeks after direct contact with an infected lesion.
Although these lesions are most often observed in men on the distal penis, they can be located in almost any place where direct contact with the infected person's lesion might occur and, although sometimes unnoticed, can be found in the female vagina and cervix, in and near the rectum, in the mouth, as well as on other potentially exposed body parts such as the fingers and neck. Genital ulcers mimicking tumors are most commonly caused by genital herpes, but can be caused by chancroid, trauma, fixed drug eruptions, and dermatologic processes.
Without treatment, after a period of 3-6 weeks, primary lesions resolve spontaneously without leaving any scars. With treatment, the lesions begin to resolve within a few days.
Second stage
Secondary syphilis is the most commonly recognized clinical syndrome of this infection, particularly among women or MSM, and it is traced to lack of treatment of the internal vaginal or anogenital lesions that occurred during the first stage.
The classic manifestations of secondary syphilis are:
- the rash, which is extraordinarily variable in appearance but is generally macular and papular, painless, 1/2 cm, reddish or copper-coloured, and may involve the face, trunk, limbs, and sometimes the mucous membranes;
- lesions on the palms of the hands or soles of the feet, here not papular in character but infiltrative, a peculiarity that highlights and distinguishes syphilis from other eruptions.
In about one third of patients with secondary disease, Condylomata Lata may occur in the genital and perianal region where flat condylomata develop that are typically warty and papillomatous and are identified as eroded grayish plaques with a foul odor.
After the resolution of second-stage onset, untreated syphilis enters a latent phase in which clinical manifestations are absent and can only be detected by serologic testing.
Third stage
Latent syphilis is further divided into early and late latent syphilis, a differentiation that influences treatment decisions and partner notification recommendations.
Based on observations from the Oslo study of untreated syphilis in the early 20th century, within a year or two of the resolution of secondary manifestations of infection, about 25% of untreated people will have recurrent secondary manifestations and thus once again be potentially infectious to sexual partners.
Most of the recurrent clinical manifestations in early latent syphilis occur during the first year of latency.
After a period of years or even decades, based on data from the pre-antibiotic era, about 1/3 of people with latent untreated syphilis will have further clinical manifestations such as late neurosyphilis, cardiovascular syphilis, or gummy syphilis.
Cardiovascular syphilis most often presents as ascending aortic aneurysm formation, aortic valve insufficiency, or coronary artery disease.
Neurological involvement in syphilis
Neurosyphilis is a dreaded but poorly understood complication of infection that can occur at any time during the course of infection. Abnormalities of T. pallidum and cerebrospinal fluid (CSF) can be detected in the CNS (Central Nervous System) in a substantial proportion of patients with early syphilis, many of whom have no obvious neurological signs or symptoms.
The importance of invasion and its impact on therapeutic decision making, particularly in the early stages of infection, remains the subject of ongoing debate and research.
Clinical neurosyphilis can present in a variety of ways that are roughly related to the duration of infection, although some findings such as ocular involvement can occur throughout the course of untreated syphilis. Some individuals with secondary syphilis may present with an aseptic meningitis syndrome of headaches and mild meningism (syphilitic meningitis).
Recognition of meningovascular syphilis, in relatively young people presenting with premonitory signs or symptoms of meningovascular syphilis, offers an opportunity for treatment to prevent additional and irreversible neurological deficits due to stroke. The most common manifestations of meningovascular syphilis are hemiplegia, aphasia, or seizures related to the involvement of the middle cerebral artery or its branches.
DIAGNOSIS
Diagnosis is based on direct observation of symptoms, but can also be confirmed by microscopic analysis of samples taken from the wound or by serologic tests that look for antibodies developed against the disease.
TREATMENT
Treatment is antibiotic and is based on:
- Long-acting benzathine penicillin
- Azithromycin
- Ceftriaxone
Effective therapy tends to be based on early identification of the disease.
PREVENTION
The risk of infection drops significantly with the use of condoms in vaginal, anal, and oral intercourse. However, despite the use of contraception, the chances of contracting it are not nullified.
There are currently no vaccines available against syphilis although the global nature of the public health problem posed by this infection suggests that a vaccine could target populations of all income targets.
Prevention and control of syphilis by national, state, and local public health agencies include disease surveillance, epidemiological analysis, education of providers and the public, support for clinical and preventive services, outreach to diagnose recent patients and their sexual partners, and screening of people at high risk of infection.
Screening means assessing the presence of a disease in people without signs or symptoms of that disease; unfortunately, such programs are not organised in the Italian territory. The test is usually performed on people who have reported signs or symptoms.
Bibliography & Sitography
- Edward W Hook. Syphilis.Lancet 2017; 389:1550-57;
- Sexually Transmitted Disease Surveillance 2017. Syphilis. Centers for Disease Control and Prevention;
- Dean T. Jamison Rachel Nugent,Hellen Gelband,Susan Horton,Prabhat Jha,Ramanan Laxminarayan Charles N. Mock. Disease control Priorities, Third Edition. World Bank Group.
- Caroline E. Cameron, PhD. Syphilis Vaccine Development: Requirements, Challenges and Opportunities. HHS Public Access Author manuscript Sex Transm Dis. Author manuscript; available in PMC 2019 September 01.